Alcohol use disorder (AUD) is a chronic and progressive condition characterized by the inability to control or stop alcohol consumption despite negative consequences. It affects physical and mental health, disrupts relationships, and impairs daily functioning, making it a significant public health concern.
In the United States, approximately 14.5 million adults were diagnosed with AUD in 2022, with Pennsylvania reporting a significant prevalence rate, particularly among young adults. This disorder disrupts lives and poses considerable challenges to individuals and their families.
The main causes of alcohol addiction are multifactorial, involving genetic predisposition, environmental influences, and psychological factors such as chronic stress or trauma. Early exposure to alcohol and peer pressure also contribute to its development, increasing the risk of dependency over time.
Symptoms of AUD include a loss of control over alcohol consumption, prioritizing drinking over responsibilities, and experiencing physical and psychological dependence. These symptoms manifest in behaviors like neglecting work or relationships, cravings, and withdrawal when not drinking.
The effects of alcohol addiction are profound, ranging from physical health issues like liver disease and cardiovascular problems to mental health conditions such as depression and anxiety. Social consequences include damaged relationships, job loss, and legal troubles, further exacerbating the disorder’s impact.
Common withdrawal symptoms during recovery include tremors, seizures, sweating, anxiety, and insomnia. Severe cases lead to delirium tremens, which are life-threatening without medical supervision. Professional detox services are required during this phase to ensure safety and comfort.
Treatment options for AUD include behavioral therapies, medication-assisted treatment, and holistic approaches like mindfulness practices. Programs such as Alcoholics Anonymous and evidence-based interventions like cognitive-behavioral therapy have proven effective in reducing relapse rates and promoting sustained recovery.
The recovery process involves detoxification, early recovery, and maintenance. Long-term relapse prevention strategies, such as building a support network and adopting healthy coping mechanisms, are required for maintaining sobriety and fostering a fulfilling, alcohol-free life.
What is Alcohol Addiction (Alcohol Use Disorder)?
Alcohol addiction, clinically referred to as Alcohol Use Disorder (AUD), is a chronic condition marked by a persistent inability to regulate or cease alcohol consumption despite its adverse effects on personal, professional, and social aspects of life. This condition involves both physical and psychological dependence on alcohol, leading to compulsive drinking behaviors that are difficult to control without intervention. AUD is classified within the broader category of Substance Use Disorders (SUDs), which are mental health conditions affecting brain function, behavior, and overall well-being.
Alcohol addiction is considered a chronic and relapsing brain disorder that impacts both mental and physical health. Over time, it alters brain chemistry, fostering compulsive alcohol use. These changes are driven by both psychological and physiological factors, making it challenging for individuals to stop drinking independently. Chronic alcohol use is associated with increased dopamine release, a neurotransmitter linked to pleasure and reward. Over time, this creates a cycle of dependence. This dependence disrupts the brain’s ability to regulate neurotransmitters, leading to withdrawal symptoms such as anxiety, tremors, and intense cravings when alcohol use is reduced or stopped.
The DSM-5 defines AUD as a spectrum of problematic drinking behaviors, categorized as mild, moderate, or severe, based on the number of symptoms exhibited. These symptoms include withdrawal, cravings, failed attempts to cut back, and continued use despite negative outcomes. The time required for AUD to develop varies and is influenced by genetic predisposition, drinking patterns, and co-occurring mental health issues. Frequent binge drinking or daily alcohol use significantly increases the risk of developing dependence.
The National Institute on Alcohol Abuse and Alcoholism (NIAAA) reports that alcohol use disorder affects millions in the United States, with approximately 14.5 million individuals aged 12 and older living with AUD in 2021. Furthermore, alcohol is a leading cause of preventable death, contributing to around 95,000 fatalities annually.
Why Is Alcohol Addiction a Serious Issue in Adults?
Alcohol addiction is a serious issue in adults because it affects their ability to fulfill key responsibilities within their families, careers, and society. Adults with AUD struggle to maintain productivity at work, leading to job instability and financial strain. Within families, alcohol addiction erodes relationships, creates conflict, and negatively impacts children and dependents.
In broader societal roles, adults battling AUD face legal issues, impaired decision-making, and reduced community engagement, further compounding the disorder’s far-reaching consequences. The health risks associated with AUD, such as liver disease, cardiovascular problems, and mental health disorders, further exacerbate its impact on adults, undermining their ability to meet personal and professional responsibilities.
In the United States, AUD is a widespread issue, with approximately 14.5 million individuals aged 12 and older affected as of 2021, according to the National Institute on Alcohol Abuse and Alcoholism (NIAAA). Alcohol use is responsible for around 95,000 preventable deaths annually, highlighting its significant toll on public health.
Certain demographics experience varying prevalence rates of AUD, with non-Hispanic Whites (7.7%) being more affected than Hispanic (4.6%) or Black populations (4.5%). Men are disproportionately impacted, with nearly 9% reporting alcohol dependence compared to 5% of women. Increasing rates of binge drinking among women signal a concerning trend.
Geographically, states like New Hampshire show higher AUD rates, with approximately 8% of adults affected, compared to the national average of 6%, reflecting the influence of cultural and societal norms on drinking behaviors.
How Does Alcohol Addiction Develop?
Alcohol addiction develops gradually as repeated use leads to tolerance, dependence, and changes in brain chemistry. The process begins with casual drinking, where alcohol is consumed socially or recreationally. Over time, repeated use increases tolerance, requiring larger amounts of alcohol to achieve the same pleasurable effects.
Tolerance creates a cycle of increased alcohol consumption, where the brain adapts to the presence of alcohol by altering its neurotransmitter systems, particularly those involving dopamine and GABA, which regulate reward and relaxation. As tolerance builds, physical and psychological dependence develops.
Alcohol dependence occurs when the body and mind begin to rely on alcohol to function normally, leading to withdrawal symptoms such as anxiety, irritability, and tremors when drinking stops. This dependence reinforces compulsive drinking behaviors as individuals seek to avoid discomfort and maintain a sense of normalcy.
The amount of alcohol needed to develop addiction varies depending on genetic predisposition, frequency of use, and individual biology. For some, consistent heavy drinking over months or years leads to addiction, while others with genetic or psychological vulnerabilities develop Alcohol Use Disorder (AUD) more rapidly, even with moderate consumption.
According to a study by the National Institute on Alcohol Abuse and Alcoholism (NIAAA), titled “Drinking Levels and Patterns Defined,” consuming five or more drinks on any day or 15 or more drinks per week for men, and four or more drinks on any day or eight or more drinks per week for women causes alcohol addiction.
How Long Does It Take to Develop an Addiction to Alcohol?
It takes weeks to years to develop an addiction to alcohol, depending on individual factors such as genetics, drinking frequency, and the amount consumed. Some people develop Alcohol Use Disorder (AUD) within a few months of consistent heavy drinking, particularly if they consume large quantities regularly or engage in binge drinking. For others, the process takes several years of habitual alcohol use before dependence forms.
Genetic predisposition is also significant, as individuals with a family history of addiction are at a higher risk of developing AUD more quickly. The amount of alcohol consumed is another integral factor; those who exceed the thresholds defined by the National Institute on Alcohol Abuse and Alcoholism (NIAAA), five or more drinks daily for men or four or more for women, are at a seriously increased risk. Gradual changes in brain chemistry due to repeated use accelerate the development of tolerance, dependence, and addiction over time.
What Causes Alcohol Addiction in Adults?
The causes of alcohol addiction in adults are genetic predisposition, mental health disorders, and environmental factors. Genetic predisposition is the leading cause, with inherited traits accounting for around half of the risk for Alcohol Use Disorder (AUD). Individuals with a family history of alcohol dependence are more likely to develop similar behaviors due to genetic vulnerabilities and early alcohol exposure.

The causes of alcohol addiction in adults are as follows:
- Genetic Predisposition: Genetic factors account for 50–60% of the risk for alcohol addiction, as noted by Abel, T. in “Encyclopedia of Behavioral Neuroscience.” A parent with alcohol addiction increases the likelihood of similar behaviors in their children due to shared vulnerabilities and early exposure. Genetic traits affecting how the brain processes reward and stress make some individuals more prone to addiction.
- Mental Health Disorders: Psychological conditions like depression, anxiety, and PTSD are significant risk factors. According to the HelpGuide, up to 1/3 of people with clinical depression misuse alcohol to self-medicate emotional pain. This creates a cycle where temporary relief from alcohol worsens mental health and drives dependence.
- Environmental Factors: Growing up in a household with alcohol misuse or in a community where heavy drinking is normalized increases the risk of AUD. Adolescents exposed to frequent alcohol use are more likely to start drinking early, as highlighted by Rose RJ, Dick DM. et al. in “Gene-Environment Interplay in Adolescent Drinking Behavior.” Stressors like poverty or family conflict further act as triggers, pushing individuals toward alcohol as a coping mechanism.
- Stress and Trauma: High levels of stress, particularly from life events like job loss or personal trauma, are common triggers for alcohol addiction. Chronic stress alters brain chemistry, increasing the likelihood of using alcohol to manage emotional burdens, leading to dependency over time.
Who is at Risk for Alcohol Use Disorder?
Adults with mental health conditions, chronic stress, and a family history of alcohol use disorder are at risk of developing Alcohol Use Disorder (AUD). Those who work in high-pressure environments, such as healthcare or law enforcement, are particularly vulnerable due to chronic stress, which alters the brain’s reward system and increases the appeal of alcohol as a coping mechanism, as studied by Anthenelli R., Grandison L., et al. 2012, titled “Effects of Stress on Alcohol Consumption.”
Individuals with mental health conditions such as anxiety or depression turn to alcohol for temporary relief, which quickly leads to dependence. About 29% of people with mental illnesses abuse alcohol or drugs. This includes people with anxiety, depression, and other mental health conditions, as studied by HelpGuide.org.
Young adults aged 18–24 are also at heightened risk, particularly due to peer influence and social norms that promote heavy drinking. According to the Substance Abuse and Mental Health Services Administration (SAMHSA), early onset of drinking before age 15 increases the likelihood of developing AUD by four times compared to those who begin drinking at the legal age, as studied by Donovan JE, Molina BS. et al. 2011, titled “Childhood risk factors for early-onset drinking.”
Men are nearly twice as likely to develop AUD compared to women, with 17% of men affected versus 8% of women, as researched by White AM. et al. 2020, titled “Gender Differences in the Epidemiology of Alcohol Use and Related Harms in the United States.” However, women progress more rapidly from misuse to dependence due to biological differences in alcohol metabolism.
What Are the Symptoms of Alcohol Use Disorder?
The symptoms of alcohol use disorder are physical, emotional, and behavioral changes that progressively worsen as dependence develops. Early warning signs include increased alcohol consumption, cravings, and impaired control over drinking.
The physical symptoms of alcohol use disorder are as follows:
- Increased tolerance: As alcohol dependence develops, the body requires more alcohol to achieve the same effects. Over time, individuals need to drink larger quantities to feel the same level of intoxication, leading to increased consumption.
- Withdrawal symptoms: When a person with alcohol addiction stops drinking, they experience physical withdrawal symptoms, including sweating, shaking, nausea, and anxiety. These symptoms range from mild to severe and are dangerous if not properly managed.
- Blackouts or memory lapses: Frequent episodes of memory loss or blackouts, where the individual does not recall events, are common in alcohol addiction. This is due to the brain’s inability to store memories after excessive drinking.
- Sleep disturbances: Alcohol use, especially in large amounts, disrupts sleep patterns. Individuals experience insomnia or restless sleep, which worsens over time, contributing to physical and emotional exhaustion.
- Liver damage: Chronic alcohol consumption leads to liver damage, including jaundice (yellowing of the skin or eyes), cirrhosis, or fatty liver disease. These conditions are serious and are life-threatening if not addressed. According to Jackson W et al. 2019, titled “Alcohol-Related Liver Disease,” over 90% of individuals who drink excessively develop fatty liver (alcohol-associated hepatic steatosis), which is sometimes reversible. About 10 to 35% experience alcoholic hepatitis, and 10 to 20% progress to alcohol-associated cirrhosis, where normal liver tissue is replaced with scar tissue, permanently impairing liver function.
The behavioral symptoms of alcohol use disorder are as follows:
- Drinking in risky situations: Individuals with alcohol use disorder engage in dangerous behaviors while intoxicated, such as drinking before driving, operating machinery, or engaging in unsafe sexual activity. These actions put them and others at risk for harm.
- Neglecting responsibilities: Alcohol addiction leads to a decline in personal, professional, or academic responsibilities. Work, school, or family obligations are ignored or neglected because alcohol becomes the primary focus.
- Social isolation: As the addiction progresses, individuals isolate themselves from social activities and relationships that do not involve alcohol. This withdrawal from social circles leads to feelings of loneliness and further dependence on alcohol.
- Hiding alcohol consumption: People with alcohol use disorder engage in deceptive behavior, such as lying about how much they drink, hiding alcohol, or drinking secretly to avoid conflict or judgment.
- Legal or financial problems: Alcohol use disorder leads to legal trouble, such as DUIs or public intoxication, and financial difficulties, as individuals prioritize alcohol over other basic needs.
The Psychological symptoms of alcohol use disorder are as follows:
- Intense cravings: Intense craving is a major symptom of alcohol use disorder, which is a strong, persistent craving for alcohol. This leads to preoccupation with obtaining and consuming alcohol, making it the central focus of the individual’s thoughts.
- Anxiety, depression, and irritability: Many individuals with alcohol use disorder experience heightened anxiety or depression, especially when not drinking. These emotions become exacerbated as alcohol use continues, leading to a negative feedback loop.
- Mood swings: Alcohol addiction causes significant emotional instability, with individuals frequently experiencing mood swings, irritability, or extreme feelings of guilt or shame related to their drinking behaviors.
- Loss of interest in other activities: As alcohol consumption increases, individuals lose interest in activities they once enjoyed, such as hobbies, socializing, or work. Drinking becomes the primary source of pleasure or relief from stress.
- Paranoia and cognitive impairments: Some individuals experience paranoia, irrational fears, or delusions as a result of excessive alcohol use. Cognitive functions, such as concentration, decision-making, and memory, are also impaired.
The signs of alcohol use disorder are as follows:
- Drinking more than intended: One of the first signs of alcohol use disorder is an inability to control the amount of alcohol consumed. People drink more frequently or in larger quantities than they initially planned.
- Increased time spent drinking or recovering from alcohol use: As the alcohol addiction develops, individuals spend significant amounts of time obtaining, drinking, or recovering from alcohol. This leads to neglect of other important activities or responsibilities.
- Neglecting responsibilities: Increased alcohol use causes individuals to fail in their daily responsibilities, such as work, school, or family duties. They neglect to fulfill these obligations due to alcohol consumption becoming a priority.
- Social withdrawal: Individuals with alcohol use disorder begin isolating themselves from social situations, particularly those that do not involve drinking. This isolation contributes to feelings of loneliness and reinforces the addiction.
- Cravings or preoccupation with alcohol: A strong desire or craving for alcohol, along with frequent thoughts about drinking, is a pivotal early indicator of alcohol use disorder. These thoughts dominate the person’s day-to-day life, impacting their ability to focus on other tasks.
- Relationship problems: Alcohol use disorder causes strain in relationships with family, friends, or colleagues. Issues related to alcohol consumption lead to conflicts, misunderstandings, and a communication breakdown, further isolating the individual.

How Do AUD Symptoms Differ From Casual Drinking?
AUD symptoms differ from casual drinking in that they involve a loss of control, increased cravings, negative impacts on life, and withdrawal symptoms, whereas casual drinking does not lead to such consequences.
AUD symptoms differ from casual drinking in the following ways:
| Aspect | Casual Drinking Habits | Alcohol Addiction |
| Control | Drink in moderation, able to stop anytime | Difficulty in controlling drinking, unable to stop despite wanting to |
| Cravings | Rare or occasional cravings | Frequent, intense cravings for alcohol |
| Impact on Life | No significant effect on personal or work life | Major disruptions in work, social, and family responsibilities |
| Withdrawal Symptoms | None or mild (e.g., mild hangover) | Severe withdrawal symptoms like anxiety, tremors, nausea, and sweating |
| Drinking Pattern | Drink occasionally or socially | Regular, excessive drinking, sometimes daily |
The fundamental differences between AUD and casual drinking are the loss of control, the intensity of cravings, the negative impact on various aspects of life, and the presence of withdrawal symptoms. Casual drinking remains moderate and doesn’t interfere with daily life or cause physical dependence, whereas alcohol addiction significantly alters behavior and health.
What Are the Effects of Alcohol Addiction on Adults’ Lives?
The effects of alcohol addiction on adults’ lives include affecting physical health, relationships, work performance, and mental well-being. Chronic alcohol use leads to serious health conditions such as liver damage, cardiovascular problems, and an increased risk of cancer. It also strains relationships as communication breaks down and emotional distance grows between individuals and their loved ones. Work performance deteriorates due to decreased productivity and absenteeism, leading to job loss.
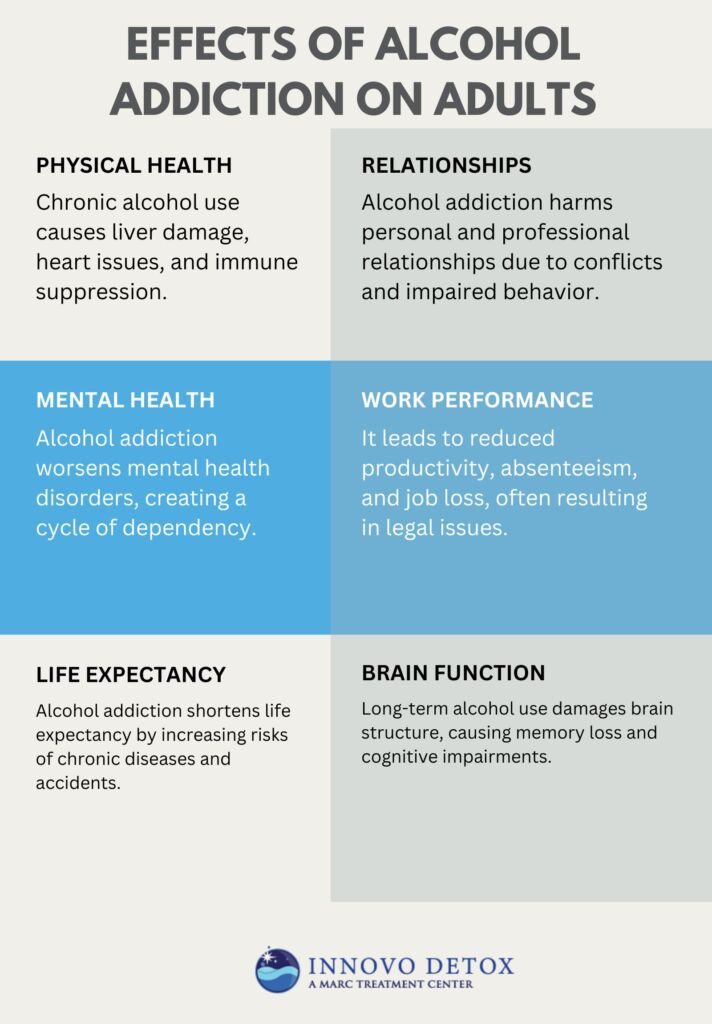
The effects of alcohol addiction on adults’ lives are as follows:
- Physical Health: Chronic alcohol use leads to severe health complications, including liver diseases like fatty liver, alcoholic hepatitis, and cirrhosis. Alcohol also increases the risk of cardiovascular problems, such as high blood pressure, heart disease, and stroke, while impairing the immune system. More than 90% of people who drink excessively experience liver damage. Around 10 to 35% develop inflammation, known as alcoholic hepatitis. About 10 to 20% of heavy drinkers progress to cirrhosis, a more severe form of liver damage, according to MSD Manual 2023, “Alcohol-Related Liver Disease.”
- Relationships: Alcohol addiction strains relationships with family, friends, and coworkers. Frequent alcohol use leads to communication breakdowns, emotional distancing, and increasing conflicts. The consequences of impaired judgment and erratic behavior alienate loved ones, and studies show that approximately 60% of individuals with alcohol dependence report significant relationship problems due to their drinking behaviors, according to research by Hutchinson DM et al. 2014, titled “The Impact Of Alcohol Use Disorders On Family Life: A Review Of The Empirical Literature.”
- Work Performance: Alcohol addiction negatively impacts work performance, leading to absenteeism, decreased productivity, and impaired decision-making. As alcohol use increases, individuals neglect professional responsibilities, resulting in job loss or career stagnation. In severe cases, alcohol addiction leads to legal issues, such as DUIs, that further damage one’s career.
- Mental Health: Alcohol addiction exacerbates existing mental health conditions and contributes to the development of new disorders. It is commonly associated with depression, anxiety, and mood swings, which in turn drive individuals to drink more as a coping mechanism. Approximately 27% to 40% of individuals with alcohol use disorder also experience co-occurring mood disorders, according to a study by Medical News Today titled “What mood disorders are associated with alcohol use disorder?” emphasizing the importance of addressing both alcohol addiction and mental health issues in treatment.
- Brain Function: Chronic alcohol use interferes with brain structure and function, leading to cognitive impairments, memory loss, and decreased brain volume. Long-term alcohol abuse disrupts neurotransmitter balance, causing mood swings, anxiety, and depression. About 30% of alcoholics develop Wernicke-Korsakoff syndrome, a severe brain disorder linked to alcohol use, which affects memory and cognitive abilities, according to an article by the National Institute on Alcohol Abuse and Alcoholism, 2021, titled “Alcohol’s Effects on Health.”
- Life Expectancy: Alcohol addiction significantly reduces life expectancy due to the increased risk of chronic diseases like liver disease, heart problems, and various cancers. Research by Westman J, Ösby U., et al. 2015, titled “Mortality and life expectancy of people with alcohol use disorder in Denmark, Finland, and Sweden,” suggests that individuals with alcohol use disorder lose up to 24–28 years of life expectancy compared to their peers without the condition, largely due to the higher incidence of alcohol-related health complications and accidents.
What Disorders Are Common Among Individuals with Alcohol Use Disorder?
The common disorders among individuals with alcohol use disorder are depression, anxiety, liver disease, and cardiovascular issues. Depression and anxiety are frequently co-occurring conditions in those with alcohol addiction, affecting 27% to 40% of individuals with AUD, according to an article by Medical News Today titled “What mood disorders are associated with alcohol use disorder?” These mental health issues exacerbate alcohol misuse as individuals attempt to self-medicate.
Chronic alcohol use leads to severe liver conditions, including fatty liver, alcoholic hepatitis, and cirrhosis, which impair liver function and are life-threatening. Individuals with AUD are at higher risk for cardiovascular diseases, including hypertension, heart disease, and stroke, due to the negative effects of alcohol on the heart and blood vessels. The study by Sung C et al. 2022, titled “Risk of cardiovascular disease in patients with alcohol use disorder: A population-based retrospective cohort study,” found that individuals with alcohol use disorder (AUD) had a higher incidence of cardiovascular disease (CVD) at 27.39%, compared to 19.97% in the control group.
Can Alcohol Addiction Be Fatal?
Yes, alcohol addiction can be fatal due to risks like alcohol poisoning, liver failure, and accidents. Alcohol poisoning occurs when the body is overwhelmed by excessive alcohol, leading to respiratory failure or coma. Chronic alcohol abuse also causes liver failure, where the liver no longer functions due to prolonged damage.
Studies indicate that alcohol-related deaths are significant, with approximately 374,197 alcohol-induced deaths in 2021, as reported by Becker T et al.2021, titled “High and Rising Mortality Rates Among Working-Age Adults.” Around 95,000 annual deaths in the United States, according to the National Institute on Alcohol Abuse and Alcoholism (NIAAA) 2024 in their report titled “Alcohol-Related Emergencies and Deaths in the United States.”
How is Alcohol Addiction Diagnosed?
Alcohol addiction is diagnosed using a combination of clinical evaluations, diagnostic criteria, and screening tools. The primary method is based on the DSM-5 criteria, which assesses the severity of alcohol use disorder (AUD) through a series of questions about alcohol use patterns, cravings, and the impact of drinking on daily life. A diagnosis is made if an individual meets at least two of the criteria within 12 months, such as the inability to control drinking, withdrawal symptoms, and continued use despite negative consequences.
Structured interviews and screening tools like the Alcohol Use Disorders Identification Test (AUDIT) also help identify problematic drinking behaviors and assess the need for treatment. These tools provide a comprehensive approach to diagnosing alcohol addiction and determining its severity.
What Are Common Alcohol Withdrawal Symptoms?
Common alcohol withdrawal symptoms are tremors, anxiety, seizures, and sweating, which range from mild discomfort to life-threatening complications. These symptoms begin within 6 to 12 hours after the last drink and peak within 24 to 48 hours, making detox a necessary period for individuals with alcohol use disorder. According to Jesse S et al. 2017, titled “Alcohol withdrawal syndrome: mechanisms, manifestations, and management,” nearly 90% of individuals undergoing detox report experiencing these withdrawal symptoms.
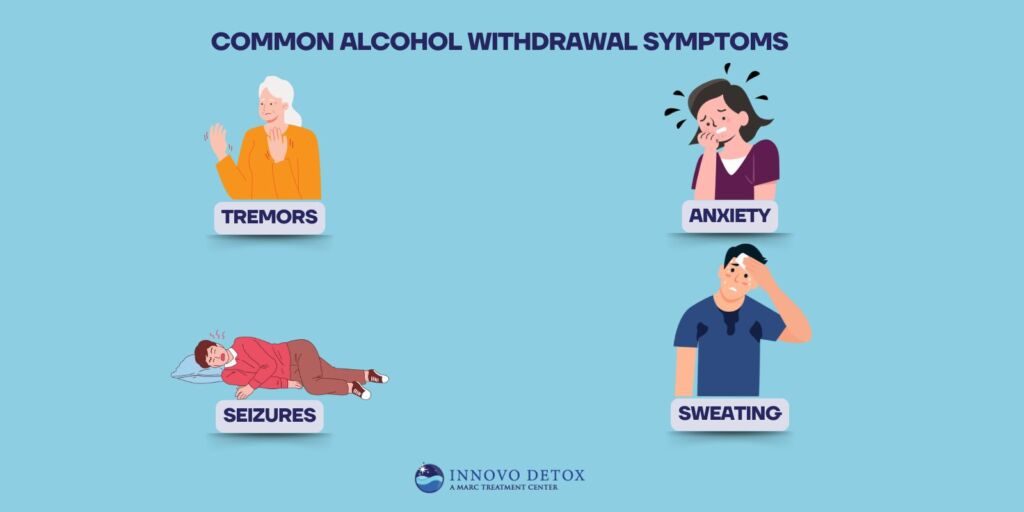
The common alcohol withdrawal symptoms are as follows:
- Tremors: Trembling of the hands and body is one of the earliest and most common withdrawal symptoms. It affects approximately 50-60% of individuals undergoing detox, accompanied by sweating and increased heart rate, according to a study by Jesse S et al. 2017, titled “Alcohol withdrawal syndrome: mechanisms, manifestations, and management.
- Anxiety: Feelings of unease and restlessness frequently occur during withdrawal. Anxiety is reported in nearly 70% of cases, reflecting the brain’s struggle to regain chemical balance after prolonged alcohol use, according to a study by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) titled “Neuroscience: The Brain in Addiction and Recovery.”
- Seizures: Severe withdrawal leads to alcohol-induced seizures, with an estimated 5-15% of individuals experiencing this dangerous symptom during detox. Most alcohol withdrawal seizures occur between 12 and 48 hours after a sharp decline in blood alcohol concentrations, as studied by Drug and Alcohol Dependence, 2022 in “Alcohol Withdrawal Seizure.” Medical supervision is important to manage these risks, as seizures are life-threatening.
- Sweating: Profuse sweating is a common physical response during withdrawal, signaling the body’s efforts to eliminate toxins. It coincides with tremors and anxiety, adding to the discomfort of the detox process.
Should You Stop Drinking Alcohol Cold Turkey?
No, you should not stop drinking alcohol “cold turkey” without medical supervision, especially if you have been drinking heavily or for a prolonged period. Sudden cessation leads to severe withdrawal symptoms, including tremors, seizures, and life-threatening complications like delirium tremens. Medical guidance ensures a safer detox process and helps manage withdrawal risks effectively.
Rapid withdrawal overwhelms the central nervous system, triggering severe symptoms such as elevated heart rate, high blood pressure, confusion, or even seizures. According to Jesse S et al. 2017, titled “Alcohol Withdrawal Syndrome: Mechanisms, Manifestations, and Management,” nearly 90% of individuals undergoing severe withdrawal develop life-threatening complications. Professional medical care provides necessary interventions, including medications and monitoring, to prevent these risks.
What Are the Treatment Options for Alcohol Addiction?
The treatment options for alcohol addiction are detox programs, behavioral therapies, medication-assisted treatment (MAT), holistic therapies, dual diagnosis treatment, and support groups. Each approach addresses physical, psychological, and social factors associated with alcohol addiction, ensuring a comprehensive recovery journey.

The treatment options for alcohol addiction are as follows:
1. Alcohol Detox Program
An alcohol detox program involves safely clearing alcohol from the body under medical supervision. Detoxification is important for managing withdrawal symptoms, stabilizing the individual, and preparing them for further treatment. Withdrawal is dangerous, with symptoms ranging from tremors to seizures, making supervised care necessary during this phase. Medical detox also offers medications to alleviate withdrawal symptoms, ensuring a safer and more comfortable detoxification process.
2. Behavioral Therapies
Behavioral therapy involves counseling techniques aimed at changing drinking behaviors and addressing the underlying psychological factors contributing to addiction. Cognitive-behavioral therapy (CBT) is effective, with evidence suggesting that individuals participating in CBT are more likely to reduce alcohol consumption and maintain sobriety.
The following are the behavioral therapies to treat alcohol use disorder:
- Cognitive Behavioral Therapy (CBT): Focuses on identifying and changing negative thought patterns and behaviors related to alcohol use. It helps individuals recognize triggers and develop coping strategies, enhancing long-term recovery outcomes. Research by Miller CB et al. 2020 titled “Feasibility and efficacy of a digital CBT intervention for symptoms of Generalized Anxiety Disorder: A randomized multiple-baseline study” indicates that CBT combined with other therapies leads to a 60% reduction in relapse rates.
- Contingency Management (CM): CM utilizes a reward-based system to reinforce positive behaviors like abstinence. A study by Higgins ST, Petry NM. et al. 1999, titled “Contingency management. Incentives for sobriety,” show that CM significantly improves treatment adherence. Research highlights CM’s effectiveness in reducing alcohol and drug use, improving treatment attendance, and promoting other goals like medication compliance and employment, making it a versatile approach in AOD disorder treatment.
- Motivational Interviewing (MI): A client-centered approach aimed at enhancing motivation to change and commit to sobriety by resolving ambivalence about alcohol use. A study by Foxcroft DR et al. 2016, titled “Motivational Interviewing for the Prevention of Alcohol Misuse in Young Adults,” found that MI had significant effects on reducing alcohol consumption, alcohol problems, and peak blood alcohol concentration (BAC) in young adults aged 15 to 24. Across 84 trials with 22,872 participants, MI showed little impact on binge drinking or risky behaviors.
- Dialectical Behavior Therapy (DBT): Effective for individuals with co-occurring mental health disorders, helping them manage emotions and reduce alcohol reliance. A study by Maffei C et al. 2018, titled “Dialectical Behavior Therapy Skills Training in Alcohol Dependence Treatment: Findings Based on an Open Trial,” involving 244 subjects found that 73.2% of the 157 patients who completed a Dialectical Behavior Therapy Skills Training (DBT-ST) program were abstinent at the program’s end. The treatment also improved emotional regulation, with outcomes independent of the initial severity of alcohol use or emotional dysregulation.
3. Medication-Assisted Treatment (MAT)
Medication-assisted treatment (MAT) for alcohol drug abuse involves FDA-approved medications to reduce cravings, minimize withdrawal symptoms, and discourage relapse. Combining medication with therapy improves treatment outcomes, according to a study by Anton RF. et al. 2008, titled “Naltrexone for the management of alcohol dependence,” indicating that individuals taking naltrexone combined with therapy are 25% more likely to remain abstinent than those who do not.
The medication-assisted treatment (MAT) for alcohol use disorder involves the following medicines:
- Naltrexone: Naltrexone works by blocking opioid receptors in the brain, which diminishes the pleasurable effects of alcohol consumption. Reducing the euphoria associated with drinking helps decrease the incentive to drink and supports individuals in maintaining abstinence. A 2022 review of 7 studies (N=1500) on injectable naltrexone for alcohol use disorder (AUD) found that treatment lasting more than 3 months reduced heavy drinking days by nearly 2 days per month. This medication is particularly beneficial for those who struggle with cravings and find it challenging to resist alcohol.
- Acamprosate: Acamprosate helps restore the chemical balance in the brain that is disrupted by chronic alcohol use. It works by modulating the activity of neurotransmitters like glutamate, which become overactive during alcohol withdrawal. By stabilizing brain function, acamprosate reduces withdrawal symptoms, helps alleviate cravings, and supports long-term abstinence. It is especially effective for individuals who have already stopped drinking and are looking for assistance in maintaining sobriety over time.
- Disulfiram: Disulfiram creates a strong deterrent to alcohol consumption by causing an unpleasant reaction when alcohol is consumed. It blocks the enzyme aldehyde dehydrogenase, leading to a buildup of acetaldehyde when alcohol is ingested. This results in symptoms like flushing, nausea, vomiting, and rapid heartbeat, making drinking physically uncomfortable. Disulfiram is most effective for individuals who are highly motivated to abstain and are looking for additional reinforcement to prevent relapse.
4. Holistic Therapies
Holistic therapies such as mindfulness, yoga, acupuncture, and art therapy complement conventional treatments by focusing on emotional and physical well-being. These approaches help reduce stress, improve self-awareness, and improve overall mental health, making them effective for sustaining recovery. Evidence from a 2021 study in the Journal of Substance Abuse Treatment found that mindfulness-based interventions reduced relapse rates by 35%.
5. Dual Diagnosis Treatment for Co-occurring Disorders
Dual diagnosis treatment addresses both alcohol addiction and co-occurring mental health conditions, such as depression or anxiety. Integrated care ensures that mental health disorders and addiction are treated simultaneously, improving outcomes. Co-occurring disorders exacerbate one another, making comprehensive treatment necessary for sustained recovery and preventing relapse.
6. Support Groups and Peer-Led Programs
Support groups, such as Alcoholics Anonymous (AA), provide a community for individuals recovering from alcohol addiction. These peer-led groups offer a platform for sharing experiences and encouragement, significantly improving motivation and accountability.
Following are the support groups and peer-led programs to treat alcohol use disorder:
- Alcoholics Anonymous (AA): AA offers a structured 12-step program that helps individuals with alcohol addiction achieve and maintain sobriety. It emphasizes personal accountability, spiritual growth, and peer support through regular meetings and sponsorship. A study by Friedman, R. 2014, titled “Taking Aim at 12-Step Programs,” has shown that participation in AA significantly increases the likelihood of long-term sobriety up to 66% by providing a supportive community and emotional connection.
- SMART Recovery: SMART Recovery is a self-empowerment program that uses cognitive-behavioral techniques to help individuals manage addiction. It focuses on practical tools for managing triggers, setting goals, and maintaining motivation. Unlike AA, SMART Recovery is non-spiritual and encourages a science-based approach to recovery. It offers flexibility and empowers individuals to take control of their addiction.
What Are the Stages of Alcohol Recovery?
The stages of alcohol recovery are detox, early recovery, and maintenance. Each stage helps individuals progress toward long-term sobriety while managing challenges.
The stages of alcohol recovery are as follows:
- Detox: The detox stage involves the initial phase of alcohol withdrawal, where the body clears alcohol from the system. This stage lasts from a few days to a week, depending on the severity of alcohol dependence. Detoxification is conducted under medical supervision to manage withdrawal symptoms, such as tremors, anxiety, and seizures, and to ensure safety. During this stage, the focus is on physical stabilization.
- Early Recovery: Early recovery is focused on establishing the foundation for long-term sobriety. Individuals work to develop healthier coping mechanisms, build a support system, and address underlying issues that contribute to their alcohol use disorder (AUD). This phase involves therapy, support groups, and relapse prevention strategies. Statistically, relapse rates during early recovery are high, with up to 40-60% of individuals experiencing relapse in the first year of recovery, according to a study by the National Institute on Drug Abuse (NIDA) et al. 2020, titled “How effective is drug addiction treatment?”
- Maintenance: In the maintenance phase, individuals work to sustain their sobriety and avoid relapse. This stage focuses on ongoing therapy, lifestyle changes, and coping mechanisms to manage triggers and stress. Long-term success in this phase requires continued involvement in support groups, such as Alcoholics Anonymous (AA), and consistent use of relapse prevention strategies. The goal is to maintain sobriety for the long term and prevent a return to addictive behaviors.
Is Total Abstinence from Alcohol Achievable?
Yes, total abstinence from alcohol is achievable, though success depends on various factors, including the severity of alcohol use disorder (AUD), support systems, and commitment to recovery. Programs like Alcoholics Anonymous (AA) have helped many individuals achieve long-term abstinence.
For some individuals, complete abstinence is not the goal, and harm reduction strategies, such as reducing alcohol consumption, are more realistic. Support systems, therapy, and ongoing treatment are key factors in maintaining sobriety or reducing harmful drinking behaviors.
What Are the Most Common Triggers for Relapse During Alcohol Recovery?
The most common triggers for relapse during alcohol recovery are stress, emotional distress, or social situations involving alcohol.
Common triggers for relapse during alcohol recovery are as follows:
- Stress: Prolonged stress, whether from work, family, or financial pressures, leads individuals to use alcohol as a coping mechanism. Chronic stress alters the brain’s reward system, making alcohol more appealing for stress relief, which increases the risk of relapse. A study by Anthenelli R, Grandison L. et al. (2012) found that stress significantly contributes to alcohol consumption relapse.
- Social Situations: Being in environments where alcohol is readily available or surrounded by people who drink heavily triggers a relapse. Social pressure or the temptation to drink at social gatherings is overwhelming for individuals in recovery. Studies show that peer influence and the availability of alcohol are significant relapse factors.
- Emotional Distress: Negative emotions like anxiety, depression, or loneliness are common relapse triggers. These emotions drive individuals back to alcohol as a form of self-medication. Research indicates that negative emotions are responsible for a significant proportion of relapse cases.
What Relapse Prevention Strategies Help Maintain Alcohol Sobriety?
Relapse prevention strategies that help maintain alcohol sobriety are identifying triggers, building a support network, practicing mindfulness, and engaging in ongoing therapy. These strategies focus on long-term recovery by fostering emotional resilience and creating a supportive environment.
Relapse prevention strategies that help maintain alcohol sobriety are as follows:
- Identifying Triggers: Recognizing personal triggers, such as stress, social situations, or emotional distress, enables individuals to avoid or manage high-risk scenarios proactively. Individuals develop tailored strategies to navigate these challenges by apprehending what increases the likelihood of relapse.
- Building a Support Network: Surrounding oneself with positive influences, such as supportive friends, family, or recovery groups, provides emotional and practical assistance during recovery. Programs like Alcoholics Anonymous (AA) offer ongoing support and accountability, creating a sense of community that bolsters long-term sobriety.
- Practicing Mindfulness: Techniques like meditation and mindfulness-based stress reduction help individuals stay present, manage cravings, and reduce stress. Mindfulness practices significantly decrease relapse risk by improving emotional regulation and enhancing self-awareness.
- Having a Structured Routine: Establishing daily routines that prioritize healthy habits, such as balanced meals, regular exercise, and sufficient sleep, fosters stability and reduces the risk of relapse. A structured routine helps create a predictable and supportive environment that reinforces recovery.
- Ongoing Therapy: Maintaining sobriety requires continued participation in therapy, whether individual or group-based. Approaches such as cognitive-behavioral therapy (CBT) assist individuals in identifying and addressing underlying issues, developing effective coping mechanisms, and preventing relapse.
- Sober Living Homes: These alcohol-free environments provide a supportive space for individuals transitioning from intensive treatment to independent living. With peer support and structured living arrangements, sober living homes have been shown to reduce relapse rates and promote long-term recovery significantly.
- Using Relapse Prevention Plans: Developing comprehensive long-term relapse prevention strategies that include managing high-risk situations, emergency contacts, and coping mechanisms equips individuals with practical tools to handle challenges. A relapse prevention plan is a proactive resource that improves preparedness and confidence in maintaining sobriety.
How Can Family Dynamics Influence Recovery From Alcohol Addiction?
Family dynamics influence recovery from alcohol addiction by shaping the emotional and social environment that either supports or hinders the recovery process. Positive family involvement, such as providing encouragement, participating in therapy, and fostering open communication, creates a supportive foundation for recovery.
Conversely, negative dynamics, such as enabling behaviors, codependency, or unresolved conflicts, perpetuate stress and relapse risks. Family roles shift due to addiction, with some members becoming caretakers or enablers, which strain relationships. Addressing these dynamics through family therapy or counseling helps rebuild healthy relationships, establish boundaries, and strengthen recovery.
How to Prevent Alcohol Use Disorder in Adults?
To prevent alcohol use disorder in adults, strategies focus on education, stress management, and promoting healthy coping mechanisms. These approaches aim to address underlying risk factors and promote resilience against alcohol misuse.
The following strategies are used to prevent alcohol use disorder in adults:
- Education and Awareness: Providing information about the risks of excessive alcohol consumption and its impact on physical and mental health helps individuals make informed decisions. Public health campaigns and workplace seminars raise awareness.
- Stress Management: Teaching stress-reduction techniques, such as mindfulness, yoga, or time management, equips individuals to handle life’s pressures without resorting to alcohol as a coping mechanism.
- Healthy Coping Mechanisms: Encouraging healthy coping mechanisms like exercise, hobbies, or seeking social support promotes positive ways to manage emotions and challenges, reducing reliance on alcohol.
How to Help Someone with Alcohol Addiction?
To help someone with alcohol addiction, it is important to approach them with empathy, understanding, and a nonjudgmental attitude. Openly express your concerns about their drinking habits and how they affect their health and relationships, encouraging honest dialogue. Offer support by researching and suggesting professional detox services, which provide a safe environment to manage withdrawal symptoms and begin recovery.Encourage them to seek treatment, whether through a professional detox service, counseling, inpatient rehabilitation, or support groups like Alcoholics Anonymous. Assist them in building a support system and creating a plan for managing triggers and avoiding relapse. Consistent encouragement and patience are important as recovery is gradual and setbacks occur.